Max D
Corvus Training Group
SHOULD YOU PULL OUT? NEEDLE DECOMPRESSION QUESTION.
Source: http://www.traumamonkeys.com/home/needled
Their seems to be a debate over whether or not to leave the catheter in place or remove it after performing a Needle Thoracentesis (needle decompression). The Committee on Tactical combat Casualty Care (CoTCCC) doesn't discuss this in their recommendations, they only specify decompression landmarks. Typically the units Senior Medical Officer determines the protocols and will set the policy on the procedure. Having taught TCCC / TECC to thousands of students over the past ten years or so and I would estimate that most medics remove the catheter upon relief of symptoms. Does that mean leaving the catheter in place is wrong? No it does not, often in tactical medicine it's not about right or wrong, it's about "what's the most appropriate thing to do right now, based on the current situation".
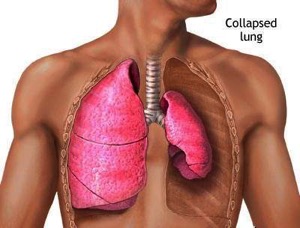
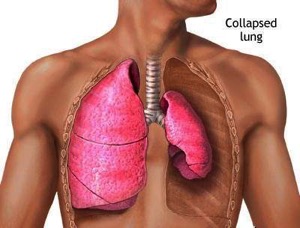
Before we discuss the pros and cons of both options, lets be clear on what's is most important. ATension Pneumothorax is a life threatening condition that requires immediate relief any discussion over the disposition of the catheter is really spitting hairs. Tension Pneumothorax continues to be the #2 cause of preventable death in combat trauma, despite the military wide acceptance of TCCC /TECC and the fact that all medics and many non-medics are provided a 14 gauge needle as well as authorization to decompress. Needle Thoracentesis is a life saving intervention but it's not typically considered a treatment, it is considered to be a diagnostic tool and a stop-gap intervention as it does not treat the underlying injury.
LEAVING THE CATHETER IN PLACE
PROS
Committees, agencies, states, rules and regulations aside here my personal opinion on the disposition of the catheter:
I remove it after I see relief of symptoms, typically after about 45 seconds and a few good breathes coupled with some manual pressure on the patients chest. That is the way I was originally taught how to do it and that's what I have stuck with, however I see nothing wrong with leaving it in place if that's what you so choose. Truthfully the disposition of the catheter is of very little consequence to me, what I'm much more concerned about is recognition of the symptoms and the life saving intervention. Tension Pneumothorax is the second leading cause of preventable combat death.1 Almost everyone is trained and provided a 14 gauge needle and we still have folks dying from a preventable injury. Why?
Why does this continue to kill patients?
Here is why I believe it continues to occur and how to solve the issue:
During training it's a simple catch, especially after a 45 minute Powerpoint on Respirations or when standing over a mannequin with latex cutouts inserted over the landmarks. Amped up, in real world emergency with a multi system trauma victim it's not always so obvious. I will put a list of the twenty or so signs & symptoms down below and I'm sure most of our readers are familiar with them, however some of them are not as common as we have been led to believe. A Tension Pneomothrax is a progressive respiratory disease. Patients are not going to initially present with a dozen symptoms, they will typically have one or two and if untreated, those symptoms will progress and it's likely more symptoms will present. Evidence suggests that patients have progressive respiratory deterioration with final respiratory arrest. The key to interpreting the early signs of hypoxia and respiratory distress is the degree of severity, but more importantly a pattern of relentless progression in a patient at risk of tension pneumothorax.4
Another important distinction to point out here is that most military medics are not carrying O2, administering O2 will have a profound impact on cyanosis, SpO2, and neurological function. Oxygen obviously benefits the patient but it does not treat the underlying problem and can mask symptoms.

- Problem -

- Solution -

Train everyone, medics included to treat patients based on what is in an Individual First Aid Kit (IFAK), not what is in a robust medical bag. A standard IFAK should have a Tourniquet, a Nasopharyngeal airway, gauze, pressure dressing, chest seals, and a 14 gauge needle. If you are treating a patient and he/she is in progressive respiratory distress, look in your IFAK and see what hasn't been utilized. If there is still a needle in the kit, then that should be your clue. If you haven't utilized your chest seals, then that should be the prompt to double-check for any holes that need to be sealed up, remembering to seal all holes regardless of size from the navel to the neck 360 degrees. A Tension Pneumothorax is an absolute life threatening conditions and if you have tried all other treatment options (recheck for holes, re-position), then it's probably time to dart.
To overcome the issue of not wanting to go Pulp Fiction and stick someone with an excalibur sized needle through the proverbial breastplate we need to continue to stress in training that an Needle Decompression is safe when performed correctly. Teach the right technique and the right location and emphasize the minimal risks associated with the procedure.
Source: http://www.traumamonkeys.com/home/needled
Their seems to be a debate over whether or not to leave the catheter in place or remove it after performing a Needle Thoracentesis (needle decompression). The Committee on Tactical combat Casualty Care (CoTCCC) doesn't discuss this in their recommendations, they only specify decompression landmarks. Typically the units Senior Medical Officer determines the protocols and will set the policy on the procedure. Having taught TCCC / TECC to thousands of students over the past ten years or so and I would estimate that most medics remove the catheter upon relief of symptoms. Does that mean leaving the catheter in place is wrong? No it does not, often in tactical medicine it's not about right or wrong, it's about "what's the most appropriate thing to do right now, based on the current situation".
Before we discuss the pros and cons of both options, lets be clear on what's is most important. ATension Pneumothorax is a life threatening condition that requires immediate relief any discussion over the disposition of the catheter is really spitting hairs. Tension Pneumothorax continues to be the #2 cause of preventable death in combat trauma, despite the military wide acceptance of TCCC /TECC and the fact that all medics and many non-medics are provided a 14 gauge needle as well as authorization to decompress. Needle Thoracentesis is a life saving intervention but it's not typically considered a treatment, it is considered to be a diagnostic tool and a stop-gap intervention as it does not treat the underlying injury.
LEAVING THE CATHETER IN PLACE
PROS
- Easy to identify that the patient may have had a Tension Pneumothorax and that a decompression was performed and may alert new providers to be on the lookout for return of symptoms.
- Easy to identify which side has been decompression was attempted on.
- Easy to determine how many times a decompression has been attempted based on the number of catheters left in place.
- Believing that it will continue to work and allow air to escape, it typically kinks and clogs and doesn't prevent the need for subsequent decompressions. If providers make this assumption they could potentially miss the return of symptoms.
- Increased risk of infection.
- If removed carefully it could potentially be used multiple times, keeping in mind that non-medics typically don't carry multiple needles. Using your only catheter once would require a non-medic to have to do subsequent decompressions with only a needle, thus increasing patient risk.
Committees, agencies, states, rules and regulations aside here my personal opinion on the disposition of the catheter:
I remove it after I see relief of symptoms, typically after about 45 seconds and a few good breathes coupled with some manual pressure on the patients chest. That is the way I was originally taught how to do it and that's what I have stuck with, however I see nothing wrong with leaving it in place if that's what you so choose. Truthfully the disposition of the catheter is of very little consequence to me, what I'm much more concerned about is recognition of the symptoms and the life saving intervention. Tension Pneumothorax is the second leading cause of preventable combat death.1 Almost everyone is trained and provided a 14 gauge needle and we still have folks dying from a preventable injury. Why?
Why does this continue to kill patients?
Here is why I believe it continues to occur and how to solve the issue:
During training it's a simple catch, especially after a 45 minute Powerpoint on Respirations or when standing over a mannequin with latex cutouts inserted over the landmarks. Amped up, in real world emergency with a multi system trauma victim it's not always so obvious. I will put a list of the twenty or so signs & symptoms down below and I'm sure most of our readers are familiar with them, however some of them are not as common as we have been led to believe. A Tension Pneomothrax is a progressive respiratory disease. Patients are not going to initially present with a dozen symptoms, they will typically have one or two and if untreated, those symptoms will progress and it's likely more symptoms will present. Evidence suggests that patients have progressive respiratory deterioration with final respiratory arrest. The key to interpreting the early signs of hypoxia and respiratory distress is the degree of severity, but more importantly a pattern of relentless progression in a patient at risk of tension pneumothorax.4
Another important distinction to point out here is that most military medics are not carrying O2, administering O2 will have a profound impact on cyanosis, SpO2, and neurological function. Oxygen obviously benefits the patient but it does not treat the underlying problem and can mask symptoms.

- Problem -
- Not recognizing the patient has developed a Tension Pneumothorax.
- Not willing to insert a 3.25" needle into a patients chest.

- Solution -

Train everyone, medics included to treat patients based on what is in an Individual First Aid Kit (IFAK), not what is in a robust medical bag. A standard IFAK should have a Tourniquet, a Nasopharyngeal airway, gauze, pressure dressing, chest seals, and a 14 gauge needle. If you are treating a patient and he/she is in progressive respiratory distress, look in your IFAK and see what hasn't been utilized. If there is still a needle in the kit, then that should be your clue. If you haven't utilized your chest seals, then that should be the prompt to double-check for any holes that need to be sealed up, remembering to seal all holes regardless of size from the navel to the neck 360 degrees. A Tension Pneumothorax is an absolute life threatening conditions and if you have tried all other treatment options (recheck for holes, re-position), then it's probably time to dart.
To overcome the issue of not wanting to go Pulp Fiction and stick someone with an excalibur sized needle through the proverbial breastplate we need to continue to stress in training that an Needle Decompression is safe when performed correctly. Teach the right technique and the right location and emphasize the minimal risks associated with the procedure.









